Sleep apnea is a sleep disorder that affects millions of people worldwide. Characterized by interrupted breathing during sleep, this condition can lead to serious complications if left untreated. Over the years, continuous positive airway pressure (CPAP) machines have emerged as the go-to treatment for sleep apnea. Let’s explore the evolution of CPAP machines and their impact on the management of sleep apnea. Understanding Sleep Apnea Sleep apnea is a complex disorder with various underlying causes. In order to grasp the significance of CPAP machines, it is crucial to understand the science behind sleep apnea and its symptoms. The Science Behind Sleep Apnea Sleep apnea occurs when the airway becomes partially or completely blocked during sleep. This obstruction can…
Category: Sleep Apnea Treatment
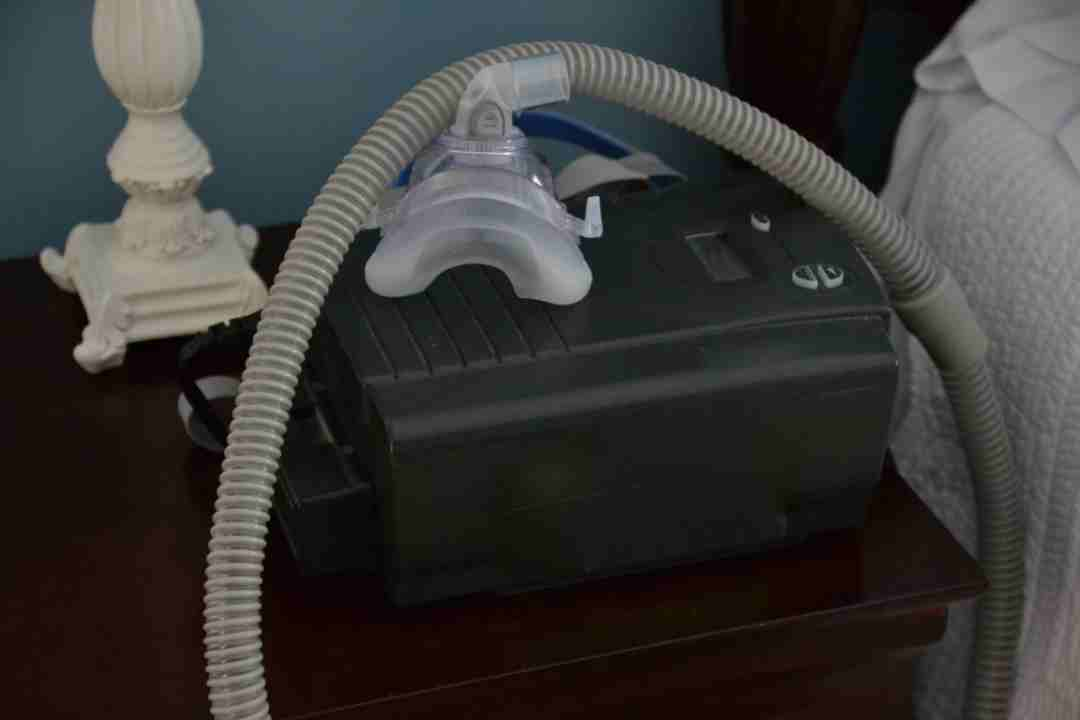
Are you struggling to get the most out of your ResMed AirSense 10 device? Do you feel like you’re not getting the quality sleep you need to feel alert and energized throughout the day? Don’t worry, you’re not alone. Many people find it challenging to navigate the various features and settings on their CPAP machine. That’s why we’ve put together this comprehensive guide to help you unlock the full potential of your ResMed AirSense 10. Let’s dive in! Understanding Your ResMed AirSense 10 Device Before we dive into the tips and tricks, it’s essential to have a basic understanding of your resmed airsense 10 device’s key features and functions. This machine is designed to deliver continuous positive airway…
As a sleep technologist, you often treat people who have sleep apnea. Continuous positive airway pressure, often known as CPAP, is an effective and well-liked treatment for sleep apnea. Patients with sleep apnea use the non-surgical technique to open up their airways while they are sleeping. According to the National Sleep Foundation, the disease affects more than 18 million Australians. The fact that the community of sleep technologists is so acquainted with the CPAP problem should thus not be surprising. Another well-known truth is how crucial it is to encourage your patients to continue their medication. In this article, we’ll examine the importance of CPAP adherence, the factors that make it difficult for patients to stick to treatment…
Although millions of people have sleep apnea, few people get it tested because they believe that snoring constantly is normal. The most prevalent kind of undiagnosed sleep apnea is called obstructive sleep apnea, or OSA. By temporarily obstructing your airway and causing you to snort while you sleep, OSA is caused by soft tissues in your throat and jaw moving backward. In addition to snoring, untreated OSA may cause additional problems. Over time, many patients begin to experience additional symptoms such recurrent headaches, brain fog, insomnia, and daytime drowsiness. They could even start performing badly on routine chores and at work. First things first If you often snore or believe you may have OSA, discuss this with your…
Even if you get enough sleep, if you often wake up with a headache or feel as if you are continually weary throughout the day, you may have a sleep disorder like sleep apnea. Sleep apnea is common and, if untreated, might have serious health consequences. As a sleep medicine specialist, it is essential to me to not only educate my patients about the potentially serious risk that sleep apnea presents to their overall health, but also to provide them the treatment options that are most appropriate for their unique situations. What is sleep apnea? When sleeping, a person with sleep apnea stops breathing. Throughout the course of the night, these pauses may happen up to 400 times…
The muscles at the back of your throat relax, which causes this to happen. The tonsils, the side walls of the throat, the tongue, and the soft palate are all supported by these muscles. These muscles also help to maintain the uvula, a triangular piece of tissue that hangs from the soft palate. Your airway narrows or possibly closes entirely when you take a breath in as the muscles in your airway loosen up. Because you aren’t getting enough air, your blood’s oxygen content may start to decline. When your brain notices that you can’t breathe, it briefly awakens you up so you can clear your airway and start breathing normally again. This epiphany often happens so quickly…